Not allowing food or drink in normal labor because of risk of rare aspiration in case you need general anesthesia isn’t evidence based care, but based on outdated hospital policy and is harmful. People in labor need and want to stay well nourished and hydrated if given the choice, instead of being then connected to an IV for at least the fluids. You are running your marathon in labor. The uterus like any muscle requires nutrients to meet its energy needs. According to research from sports medicine, it is well known that for example eating carbohydrates during exercise improves performance, reduces fatigue, and prevents ketosis. Power bars and nutrient dense snacks and hydrating fluids are given out to runners along their journey. No athlete or coach would advise performing while fasting.
When supported to labor normally and naturally, risk of emergency cesarean needing general anesthesia is very low in the healthy population. This policy of fasting before surgery began in the 1940s when general anesthesia was not as safe as today and dangerous aspiration of stomach contents was more common. These days anesthesia and airway management are much more sophisticated and improved, most cesareans don’t use general anesthetics, fasting in labor doesn't guarantee an empty stomach anyway and could lead to harmful acidic stomach juices if aspirated, and aspiration causing severe lung disease & death is extremely rare today in healthy people. Free standing birth centers and homebirth midwives do not have this no intake by mouth ’NPO’ policy.
But if you are healthy and birthing in the hospital, you can absolutely allow yourself the food and drink you need. It's your body, your birth and they don’t have authority over you. Best to discuss your preferences with your provider beforehand, in pregnancy, for if they don't support you, they may not support your other plans and you might want to change providers to those who practice evidence based care & are more in alignment with your philosophies. If you choose to stay with a provider and setting that does not allow food and drink, next option is to sneak it in, and ingest them in privacy (which might mean when you are in the bathroom).
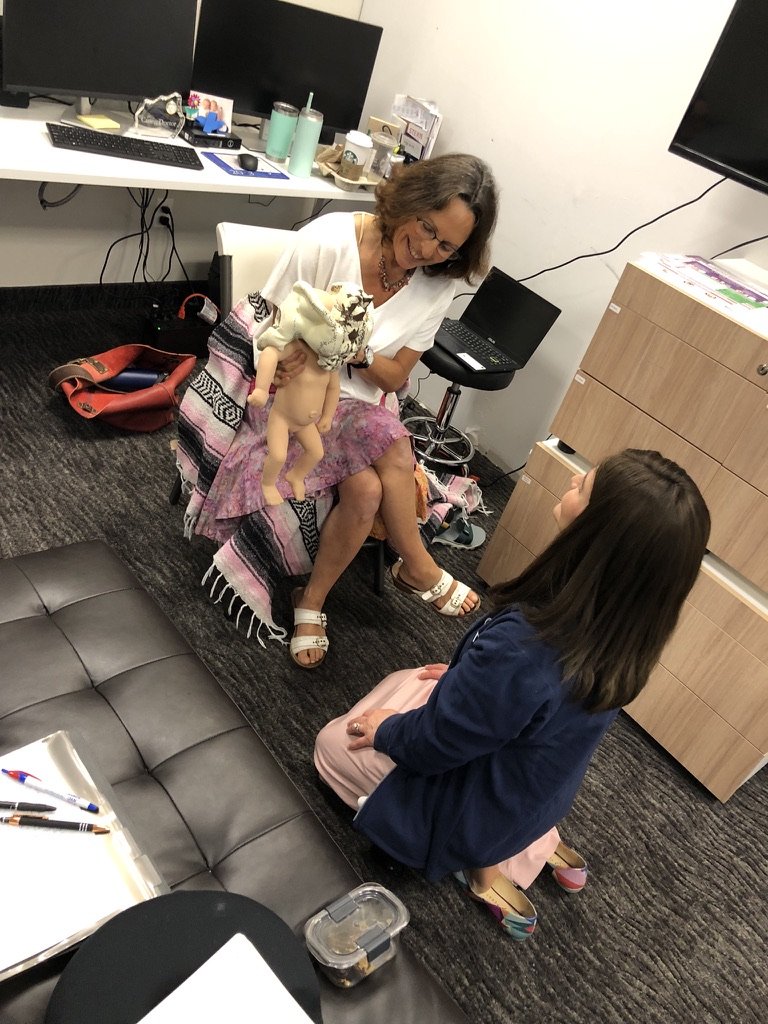
Got to stay well nourished and hydrated in labor like running your marathon.
Best labor foods are basically - whatever you want that’s nourishing and easily tolerated! Mamas tend to prefer more bland foods but not always. But you do need lots of extra quality fuel in your tank for your journey. Some favorites include organic eggs, whole grain toast and dairy or nut butter, whole grain crackers and cheese, whole grain cereal or oatmeal and dairy or nut milk, maple syrup/honey, power and granola bars, nuts and dried fruit, trail mix, dark chocolate, frozen fruit bars, fruit that’s not messy to eat.
Best drinks include water, fruit juices, herbal tea with honey, bone or miso soup broth, coconut water, smoothies, organic Gatorade, homemade labor-aid - recipe in my Natural Birth Secrets book 2nd edition.
Many who labor in hospitals that don’t allow food and drink, need IV to prevent dehydration which can cause complications needing more interventions….unless you are sneaking enough food and drinking plenty orally. If you’re pregnancy and labor are healthy are proceeding naturally, IV fluids aren’t at all necessary and may cause harm. Even the American College of Obstetricians & Gynecologists, the American Society of Anesthesiologists and of course the World Health Organization all recommend encouraging oral fluids instead of IV. Why is this not happening? Routine IV can over hydrate and decrease newborn weight and blood sugar and cause maternal swelling - even in the breasts which impairs breastfeeding, can be uncomfortable, get inflamed, infiltrated or cause infection. IV restricts needed movement in labor, undermines mama’s confidence and sense of feeling empowered and healthy. I’ve posted before on the harmful practices of restricting needing nourishment and hydration. As long as you are keeping well hydrated by drinking, you can absolutely feel no qualms about declining that routine IV.
There is also no evidence to support the IV access called saline lock for low risk laboring mamas because in case of postpartum hemorrhage. The risk of that in this population is low, & needing treatment beyond natural remedies & medications without IV even lower. An excellent practitioner can start an IV in that rare emergency.
More details in my Online Guide to Pregnancy, Childbirth & Postpartum- sold separately or discounted bundle. I’ve taken everything I’ve learned, trained, and supported women locally for over 28 years in my private practice and I’ve poured all of my love, passion, knowledge, and experience into creating something truly special for you… my new and updated Love Your Birth Pregnancy, Birth & Postpartum Guides. Same Beloved Content Plus Over 20 Added Bonus Videos! Buy Here Now!
They can be used via the mobile App or on your desktop! It’s the most up to date combination of Love Your Birth and Walk With Anne for Mamas online courses at a cheaper price! And they have an option for direct access to me for your questions and concerns!!
Whether you’re an experienced or new parent, there are hours of videos, workbooks, and PDFs to answer all of your questions. Everything is searchable, so you can just type or talk and it’ll bring you right to the exact moment in the video where I answer your question. It’ll blow your mind! If English is not your strongest language, you can even change the captions or even the audio to the language you prefer. You can get the online comprehensive prep course Love Your Birth Prenatal, Birth & Postpartum Guides - ALL of the guides for a limited-time offer of 50% off -> RIGHT HERE!
The key to a positive birth is feeling confident, strong, relaxed, and empowered during the entire process, regardless of the twists and turns it may take. I give my full heart and all I know in everything I do to support Mommas.